Two University of Miami researchers have uncovered a novel treatment that could stop COVID-19 in its tracks and help those suffering from the disease to recover.
A therapeutic called Spikenet, created by Miller School of Medicine obstetrician gynecologist Dr. Michael Paidas and assistant research professor Arumugam Jayakumar, works by blocking the novel coronavirus from entering cells in the body, where it typically replicates and spreads.
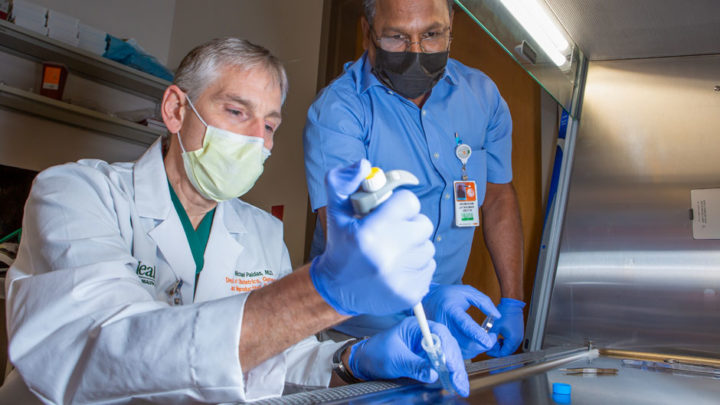
Dr. Michael Paidas and research professor Arumugam Jayakumar work to develop a compound that could block the SARS-CoV-2 virus from being able to enter human cells. Image credit: Jorge Perez/University of Miami
“Even with more vaccines available, the cases and death rates of COVID-19 have still skyrocketed, and new variants continue to emerge. So, the vaccine and treatments we have now are not enough,” said Paidas, a maternal fetal specialist who chairs the Department of Obstetrics, Gynecology, and Reproductive Sciences. “Doctors need some other options when a patient already has COVID-19, and we are desperate for this sort of therapeutic.”
Early in the pandemic, Paidas and Jayakumar were interested in finding a way to stop the SARS-CoV-2 virus, which causes COVID-19, from affecting pregnant women. They began by using advanced computer imaging to model how the virus enters the body and focused on how the SARS-CoV-2 spike protein attaches to the outside of each human cell in a process called “binding.”
Soon after, Paidas recalled an experience working with another virus, which helped him realize that it could be possible to prevent the entire binding process from starting. More specifically, the researchers saw that they might be able to create a small peptide—or a string of amino acids—that would attach to the spike protein protruding from the virus’ outer membrane. This peptide could then effectively create a “net” to blanket the spike protein, thwarting the SARS-CoV-2 virus from ever entering human cells. Because of this visual, they named the therapeutic, “Spikenet.”
“When we saw the spike protein’s structure, we realized that we could create a small protein to exquisitely bind to it,” said Jayakumar, an experienced biochemist and neuroscientist.
“Our thought was if you can stop the spike protein from binding, it’s like preventing the key from going into the lock, so you can’t open the door. And if we could prevent the virus from entering the cells, the ball game would be over,” Paidas added.
Within weeks, the pair crafted a peptide recipe that they believed would attach to the spike protein “like superglue” to prevent the virus from binding and entering human cells. They then utilized an animal model of a virus that mirrors SARS-CoV-2—which Paidas and Jayakumar also developed—and treated some of the infected rodents with Spikenet. They gave just three doses of Spikenet to the animals, over a period of six days. But the results were promising—80 percent of the rodents that received Spikenet survived their bout of COVID-19.
“At a clinical level, what’s really important is treatment of COVID-19 during the first few days when you get sick. Because if you don’t turn the corner right away, it’s a downward spiral and it’s often hard to recover,” Paidas said. “Yet in our first animal model, we saw significant survivorship early on.”
Then, Paidas and Jayakumar went a step further. They sent Spikenet to Northern Arizona University, which has a Biosafety Level 3 laboratory, something that is unavailable in Florida. There, the peptide was given as a treatment to mice infected with live SARS-CoV-2 virus. The health of most of the 20 mice who received Spikenet improved significantly. They are still analyzing the data but are elated by the initial results.
Along with survival rates, the duo discovered other benefits of Spikenet. For example, it reduces inflammation and oxidative stress levels in rodents who received the treatment. In addition, Paidas said they looked at the rodents’ water channels—or aquaporins, which regulate water in the body—and noted that these also improved with the Spikenet treatment. These are major hurdles for patients suffering with severe COVID-19, whose lungs often fill up with fluid, Paidas pointed out.
In addition, Spikenet could offer production advantages, according to the researchers. While the most common treatments for COVID-19 available today are dexamethasone, a common steroid; Remdesivir, an antiviral limited to hospitalized patients; and Regeneron, a combination of two different monoclonal antibodies that must be infused in a patient shortly after the onset of COVID-19, Spikenet may be easier to mass produce because it can be created quickly in a lab. It can also be modified for variants. Paidas and Jayakumar anticipate that Spikenet would be an injectable treatment but explained that it could potentially take other forms in the future—like Merck’s new COVID-19 pill, molnupiravir, an investigational drug given orally, or Pfizer’s new oral drug, Paxlovid.
“We are talking about a small peptide that’s easy to make, and it has all these other positive effects that are important for treating this disease and possibly others,” Paidas said.
And while the project began as a way to simply help patients, the journey to create a solution for those who are infected with COVID-19 has become personal. Not only did Paidas lose his father to COVID-19, along with a beloved University obstetrician gynecologist in his department, Jayakumar has lost eight relatives to the illness.
“We will develop Spikenet for everyone, but I especially want a treatment for pregnant moms,” Paidas said. “We hope that this will be one part of the armamentarium to treat this disease.”
In the meantime, Paidas acknowledged that the duo is working on starting some dosing studies with animals and publishing a paper about their work with Spikenet. He hopes that they can quickly find a private company to help them begin testing Spikenet in humans battling COVID-19.
“We have such a positive signal that we are meeting with pharmaceutical companies to make sure we have the most expeditious route to humans, and we hope to be in clinical trials in a range of months,” Paidas said.
Source: University of Miami
