Multiple sclerosis is a demyelinating autoimmune disease targeting brain tissues. Self-reactive T lymphocytes targeting brain-associated antigens play a major role in the pathogenesis of multiple sclerosis. Standard treatment of multiple sclerosis patients is based on nonspecific (nonselective) immunosuppressants/immunomodulators, such as hormones, interferons and others, which are, indeed, incapable of interrupting immunopatological events underlying the disease and are frequently associated with serious side effects.
Autologous T-cell vaccination exploits natural immunoregulatory mechanisms of patients aiming to achieve a selective inactivation of pathogenic autoreactive Т lymphocytes. A total of 32 patients with remittent multiple sclerosis were enrolled in a clinical trial. As shown in Figures 1 and 2, T-cell vaccination dramatically reduced the exacerbation rate and significantly improved the neurological status in patients during the first 2 years after treatment (P <0.05).
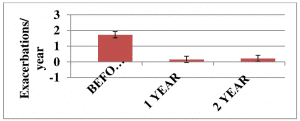
Figure 1. The exacerbation rate in patients (n=32) with remittent multiple sclerosis before and after immunotherapy onset.
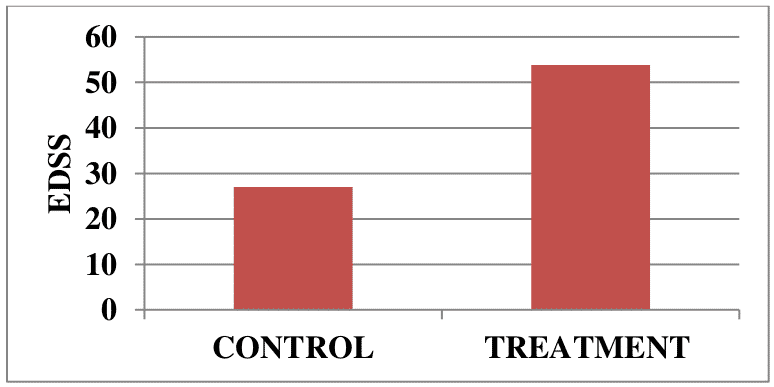
Figure 2. Neurological status in patients (n=32) with remittent multiple sclerosis before and at 2 years after immunotherapy onset.
Disease stabilization and/or neurological improvements were documented in 29/32 (~90%) patients from the treatment group, while disease progression was observed only in 3/32 (~10%) patients.
A total of 39 patients with progressive secondary (chronic) multiple sclerosis were enrolled in another clinical trial. Disease progression was stopped in 21/39 vaccine-treated patients (53.8%), compared with 6/22 (27%) control patients with no signs of disease progression, during a 2 year follow-up. Neurological improvements were detected in 5 vaccinated patients and none in the control group.
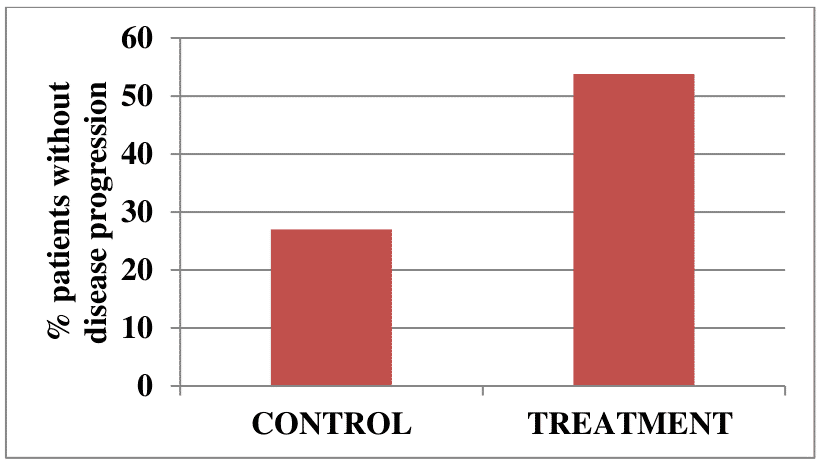
Figure 3. Percent of patients with chronic multiple sclerosis with no signs of disease progression over 2 years in the treatment and control groups.
Overall, our clinical data suggests that the nervous system of multiple sclerosis patients retains certain regenerative potential that can be activated when disease progression is stopped. We also conclude that autologous T-cell vaccination could be clinically effective in early and advanced stages of the disease.
